- Emergency Ambulance Services
- 8606811111
- 0471-4077777, 0471-7177888
- gro@sutpattom.com
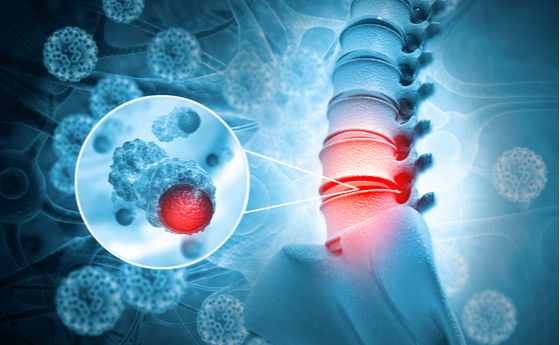
Current Concept in Management of Bone Tumours
Dr. Subin Sugath, Orthopaedic Oncosurgeon SUT Hospital, Pattom
The ability of a cell to overcome apoptosis or programmed cell death makes it cancerous. Such cell arising from mesenchymal tissue like bone give rise to bone tumours. Bone tumours are rare forming less than 2% of all malignancies. Primary bone tumour commonly affect children in their second decade while secondary bone tumours commonly affects the elderly. Benign primary bone tumours like the osteochondroma, osteoid osteoma and chondoblastoma generally affect children before skeletal maturity. Giant cell tumour which is a benign but locally aggressive tumour commonly affects patients in the third and fourth decade with a female preponderance. Primary malignant bone tumours like Osteosarcoma and Ewings sarcoma commonly affects children in the first two decades while Chondrosarcoma commonly affects patients in their 30’s and 40’s.
The most important step in managing a bone tumour is reaching a correct diagnosis before starting treatment. This is possible by doing a biopsy after doing all the required hematological and radiological investigations for that tumour. Though technically a simple procedure biopsy plays a very crucial role in the management of bone tumours as poorly done biopsies will make an otherwise salvageable limb non salvageable. Ideally biopsy must be done at those centres which are going to do the definitive procedure as they can plan their biopsies in such a way that it doesn’t jeopardize the final definitive procedure. Though open biopsies yield more amount of material for histopathology, they are associated with more complications. A simple, technically easier and associated with practically no complication is a technique called needle biopsy done with Jamshedi needle under local anesthesia. One needs to have an expert pathologist to give the correct diagnosis with needle biopsies.
Benign bone tumours can be treated by less aggressive procedures like intralesional or marginal procedures. Giant cell tumours which commonly affects the knee joint can be treated by intralesional extended curettage and bone grafting. A large cortical window is made to completely expose the tumour within the bone and the lesion is curetted out taking care not to leave behind any tumour tissue. The cavity that is left behind is filled with bone grafts, either autograft or allograft and at times with bone cement. This procedure has the advantage that the natural knee joint is preserved. The commonest complication of this procedure is recurrence of the tumour which can be treated by recurettage. At times patients present late with large tumour which have to be resected and replaced by prosthesis. Malignant bone tumours have the characteristic of spreading to other parts of the body, the lungs and other bones being the commonest sites. So a CT scan of the chest and a Technitium99 bone scan need to be done to rule out metastasis before starting treatment.
For Osteosarcoma and Ewings Sarcoma chemotherapy combined with surgery forms the main course of treatment. After 2-3 cycles of neoadjuvant chemotherapy patient is taken up for surgery. Intralesional or marginal procedures are contra indicate in malignant bone tumours. Wide resection of the tumour is a must to prevent local recurrence. Amputation used to be the treatment of choice before the 1990’s.
But with the use of more potent chemotherapeutic drugs, better imaging modalities like high resolution MRI and improved surgical techniques we have move from the era of amputation to the era of limb salvage. Here instead of the affected limb only the affected bone is resected with wide margins. An endoprosthesis is used to bridge the bone defect after tumour resection. The patient is able to do all activities of ADL except squatting on the floor. These implants cost anywhere between Rs. 60,000 to Rs. 1,00,000 depending on the length of tumour resection. There are more expensive imported implants ranging from 3 to12 lakhs which are biomechanically better. Depending on the extend of the lesion at times we may need to remove the entire bone and replace with implant as in case of Total Femur or Total Humeral replacement.
However expensive or sophisticated the implant may be it is bound to fail at some time or other. We are yet to develop an implant which is as good as our natural joint. So wherever possible one needs to take steps to preserve the natural joint by doing biological reconstruction techniques. For tumours which do not cross the growth plate, intercalary resection is possible to attain wide margins. The bone gap can either be bridged by allograft from bone bank if facilities are available. The other option would be to give high dose radiotherapy (50 Gy single shot) to the resected bone so that it kills all the tumour cells. The bone is thoroughly cleaned and reimplanted into the patient and stabilized by a platte fixation. There are enough publications in literature to show that Extra Corporeal Radiotherapy(ECRT) is a safe procedure and is not associated with local recurrence.
Pelvic tumours require multidisciplinary team approach due its complex anatomy and proximity to vital structures. Internal hemipelvectomy where different parts of the pelvis are removed depending on the tumour involvement helps to preserve the lower limb. The reconstructive technique after tumour depends on the age of the patient and type of resection. These are complex surgical procedures which take time and require multidisciplinary team approach for complete tumour excision. For tumours of the sacrum a combined anterior abdominal and posterior approach may be required. External hemipelvectomy for very large tumours requires removal of the whole limb along with the pelvis.
With the use of the newer potent chemotherapeutic drugs the life expectancy of these patients has increased from the dismal 20 – 40% to the current 60-80%. Even the simplest of procedures like biopsy is very crucial as, if it is not properly done will affect the overall outcome of treatment. Orthopaedic oncology must be a team approach where everyone combines their skill to help these unfortunate patients. If diagnosed early and treated appropriately one can get gratifying results in the management of bone tumours.